Diabetic foot ulcers progress through several stages, beginning with skin redness and irritation, often due to pressure or minor injuries. As the ulcer develops, it can lead to open sores that may not heal easily due to poor blood circulation and nerve damage common in diabetes. If untreated, the ulcer can deepen, affecting underlying tissues and potentially leading to infections, which can escalate into severe complications. Early detection and proper care are crucial to prevent the progression of diabetic foot ulcers.
What is Diabetic Foot Ulcer?
A diabetic foot ulcer is a serious and common complication of diabetes, characterized by an open sore or wound that typically occurs in about 15% of people with diabetes. These ulcers are most commonly found on the bottom of the foot and are often the result of a combination of factors including poor blood circulation, nerve damage (neuropathy), and prolonged pressure on certain areas of the foot. The reduced ability to feel pain or discomfort due to nerve damage means that even minor injuries or blisters can go unnoticed and untreated, eventually leading to the formation of ulcers. If not properly managed, diabetic foot ulcers can become infected, leading to severe complications such as tissue necrosis, gangrene, and in extreme cases, the need for amputation. Early detection and comprehensive care are crucial in managing diabetic foot ulcers, highlighting the importance of regular foot inspections and proper diabetic management to prevent their occurrence.
Signs and Symptoms of Diabetic Foot Ulcer
Diabetic foot ulcers often present with a range of signs and symptoms that should be carefully monitored, especially in individuals with diabetes. One of the early indicators is swelling or pain in the foot, which may be accompanied by any noticeable changes or discoloration in the skin or toenails. This discoloration can range from subtle darkening to more pronounced redness or blueness, signaling compromised blood flow or infection. Another common symptom is the recurrent formation of corns and calluses, which may develop into sores if left untreated. These areas of thickened skin are often the result of repeated pressure or friction, which can lead to the breakdown of the skin and the formation of ulcers. Frequent bleeding from a particular region of the foot is also a warning sign that should not be ignored, as it indicates the presence of an open wound that may not be healing properly.

Additionally, any kind of discharge, whether serous (clear fluid) or pus, is a significant indicator of infection and requires immediate medical attention. Recognizing these signs early and seeking prompt care is essential in preventing the progression of diabetic foot ulcers and avoiding serious complications.
Stages of Diabetic Foot Ulcer
Foot ulcers, particularly in individuals with diabetes, progress through several stages, each requiring careful attention to prevent worsening complications. The initial stage often begins with the development of calluses or blisters due to pressure or friction, which, if unnoticed or untreated, can lead to skin breakdown. As the ulcer advances, it penetrates deeper into the skin layers, forming an open sore that may not heal easily due to poor blood circulation and nerve damage. At this stage, the ulcer becomes vulnerable to infection, which can manifest as increased redness, swelling, warmth, and possibly pus discharge. Without proper management, the infection can spread to deeper tissues, including muscles and bones, leading to more severe complications such as cellulitis or osteomyelitis. In the most advanced stages, untreated foot ulcers can result in gangrene, where tissue death occurs due to a lack of blood supply, potentially leading to the need for amputation. Early detection and appropriate care at each stage are crucial in preventing the progression of foot ulcers and ensuring better outcomes for those affected.
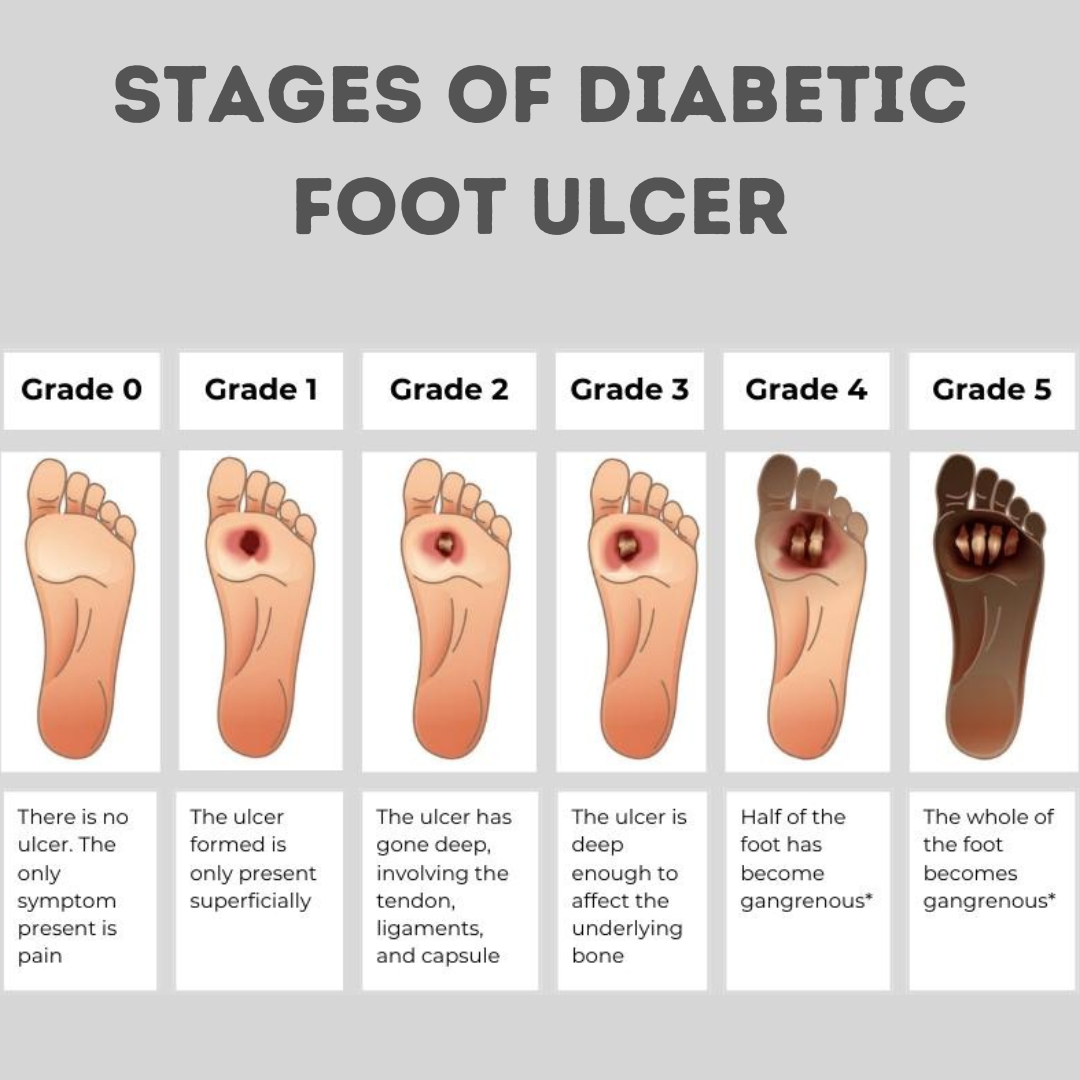
Stage 1: Normal Foot – In the first stage of a foot ulcer, the foot appears normal with no visible changes, but pain may occur intermittently. This pain can be a subtle warning sign, indicating the beginning of pressure points or minor injuries that could lead to further complications if not properly managed.
Stage 2: At-Risk Foot – At this stage, the foot is considered “at-risk” due to underlying conditions such as nerve damage (neuropathy) or reduced blood flow, both of which are common in individuals with diabetes. Your doctor will assess these risk factors, as they significantly increase the likelihood of developing a diabetic wound. Identifying these issues early on is crucial in preventing the progression to an ulcer.
Stage 3: Early Ulcer Development – In the third stage, the focus shifts to reducing pressure on the foot, which is essential to prevent the ulcer from worsening. Customized footwear is often recommended to alleviate pressure points, and proper wound care, along with bed rest, is necessary to avoid the spread of infection. These measures are vital in controlling the ulcer and preventing further damage.
Stage 4: Advanced Ulcer with Infection – By stage four, the ulcer has advanced to the point where hospitalization may be required. A culture from the wound will be taken to identify the specific bacteria causing the infection, allowing the doctor to select the most effective antibiotic. In some cases, surgical intervention, such as incision and drainage, may be necessary to control the infection and promote healing.
Stage 5: Gangrene Foot – The final stage is marked by gangrene, where blood circulation to the affected area is severely compromised, leading to tissue death. This stage requires prolonged hospitalization, intravenous antibiotics, and regular debridement to remove dead tissue. If the infection is extensive and blood circulation cannot be restored, amputation may be necessary to prevent the spread of the infection and to save the rest of the foot.
Treatment for Diabetic Foot Ulcer - Dr. Amsaveni
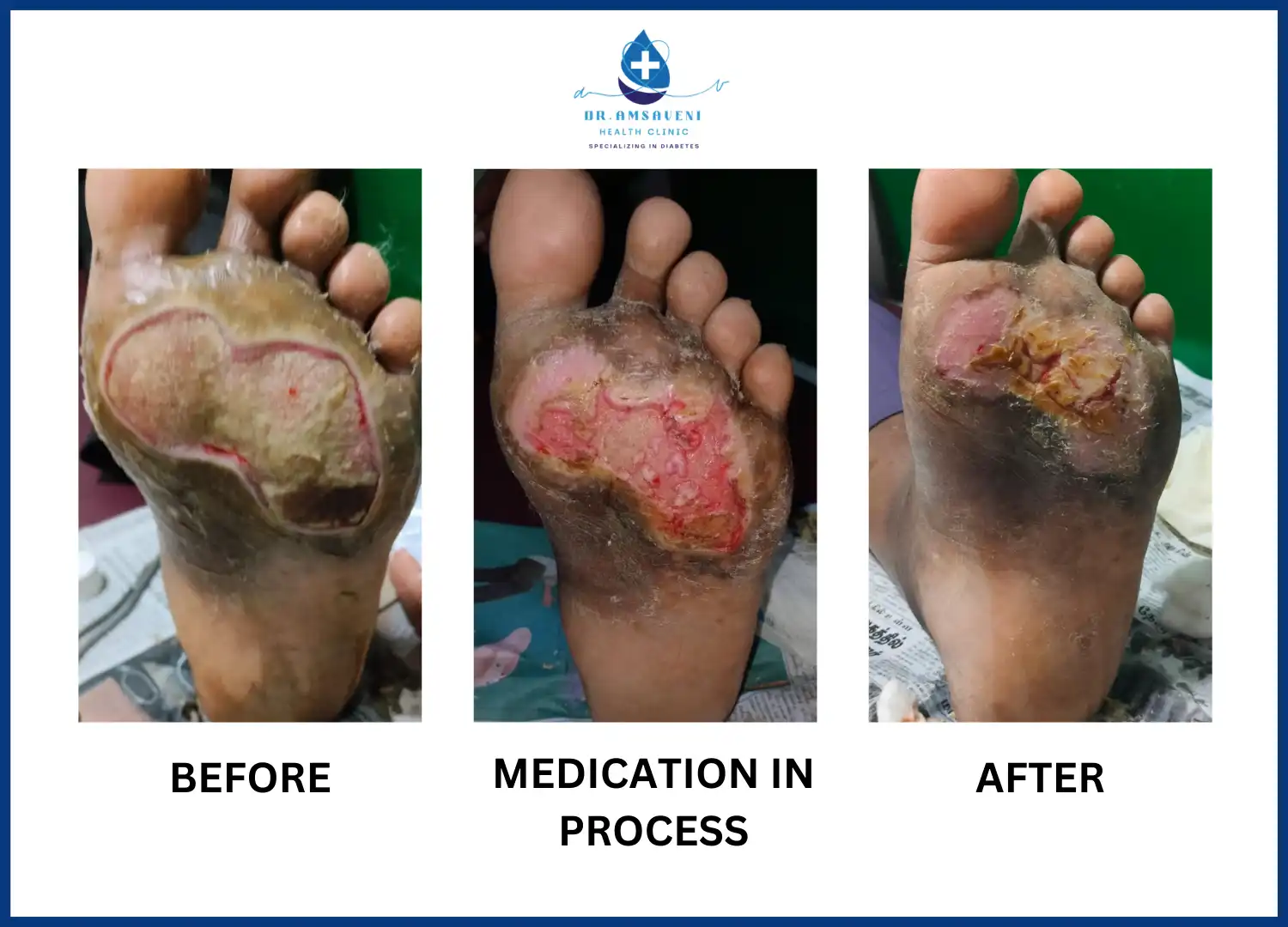
Dr. Amsaveni, a leading expert in diabetic foot ulcer treatment, specializes in non-surgical methods that focus on advanced dressing techniques and meticulous hand procedures to promote healing. Her approach is designed to address the unique challenges of diabetic foot ulcers, which often require delicate and precise care due to poor circulation and nerve damage common in diabetic patients. Dr. Amsaveni uses state-of-the-art dressings that not only protect the wound but also create an optimal environment for healing. By carefully monitoring the wound and making adjustments as needed, she ensures that the ulcer heals effectively without the need for surgical intervention. Her hands-on techniques, combined with her expertise in wound care, have successfully helped many patients recover from diabetic foot ulcers, reducing the risk of complications and improving their overall quality of life.
Successful Treatment for Diabetic Foot Ulcer - Dr. Amsaveni
Dr. Amsaveni has effectively treated diabetic foot ulcers using only advanced dressing techniques and meticulous hand procedures. These non-surgical methods, captured in images, showcase her expertise in promoting healing while avoiding invasive interventions. Through careful dressing and precise manual care, Dr. Amsaveni has helped numerous patients achieve significant recovery, demonstrating the power of skilled, non-surgical treatment in managing diabetic foot ulcers.





Diabetic Foot Ulcer - Conclusion
Diabetic foot ulcers, a serious complication of diabetes, progress through distinct stages, each requiring vigilant care to prevent worsening outcomes. These ulcers often begin with subtle symptoms, such as pain or skin changes, and can advance to severe stages involving infection, tissue death, and, in the most critical cases, gangrene. The primary causes include poor circulation, nerve damage, and excessive pressure on the foot, all of which are common in diabetic patients. Effective treatment, such as that provided by Dr. Amsaveni, focuses on early detection, reducing pressure, and employing advanced dressing techniques and non-surgical procedures. Through comprehensive care and timely intervention, these treatments can prevent the need for amputation and significantly improve patient outcomes, highlighting the importance of managing diabetic foot ulcers with expertise and attention to detail.















